ABSTRACT
Background: Vitamin D deficiency during pregnancy represents a critical global health challenge with far-reaching consequences for maternal and fetal health outcomes. Despite India's geographical advantage of receiving abundant sunlight throughout the year, vitamin D deficiency paradoxically remains highly prevalent among pregnant women across various regions, contributing to increased risks of preeclampsia, gestational diabetes mellitus, preterm birth, low birth weight, and long-term developmental complications in offspring. The complex interplay of cultural practices, lifestyle factors, dietary patterns, and physiological variations creates unique challenges in addressing this preventable nutritional deficiency. Limited comprehensive research exists from South Indian populations, particularly from teaching hospitals serving diverse demographic groups, highlighting critical knowledge gaps that must be addressed to develop effective, context-specific interventions and evidence-based public health policies.
Objective: This study aimed to determine the prevalence of vitamin D deficiency among pregnant women attending a tertiary care teaching hospital in North Coastal AP in South India and to comprehensively evaluate associations between vitamin D status and multiple determinants including sociodemographic characteristics (age, education, socioeconomic status, residential location), clinical parameters (gestational age, pre-pregnancy BMI, reproductive history), lifestyle factors (sunlight exposure patterns, clothing practices, dietary habits, physical activity), and compliance with routine supplementation protocols. Additionally, the study sought to identify independent risk factors through multivariate analysis and generate evidence-based recommendations for enhanced screening, prevention, and treatment strategies tailored to regional populations.
Methods: A comprehensive hospital-based cross-sectional study was conducted among 230 carefully selected pregnant women in their third trimester (≥36 weeks gestation) attending the Obstetrics and Gynecology Department at GIMSR Hospital, Visakhapatnam, between October 2022 and March 2024. Participants were recruited through systematic random sampling to ensure representative population coverage. Extensive data collection involved administration of structured, validated questionnaires through trained personnel, capturing detailed information on demographics, lifestyle factors, dietary patterns, supplementation compliance, and clinical parameters. Comprehensive anthropometric measurements were obtained using standardized protocols. Skin pigmentation was assessed using the internationally validated Fitzpatrick Skin Type Classification system. Serum 25-hydroxyvitamin D [25(OH)D] concentrations were measured using high-precision electrochemiluminescence immunoassay (ECLIA) technology with rigorous quality control measures. Vitamin D status was categorized according to Endocrine Society guidelines: deficient (<20 ng/mL), insufficient (20-29 ng/mL), or sufficient (≥30 ng/mL). Statistical analysis employed SPSS version 25.0 with appropriate univariate and multivariate techniques, including chi-square tests for categorical variables, t-tests for continuous variables, and logistic regression for risk factor identification.
Results: The study revealed an alarmingly high prevalence of vitamin D deficiency affecting 76.1% (n=175) of pregnant women, with an additional 21.7% (n=50) demonstrating insufficient levels, leaving only 2.2% (n=5) with adequate vitamin D status. The mean serum 25(OH)D concentration was critically low at 14.23 ± 8.33 ng/mL, with values ranging from 1.1 to 52.0 ng/mL, indicating widespread severe deficiency across the study population. Vitamin D deficiency demonstrated strong statistical associations with limited sunlight exposure patterns (p<0.001, χ²=178.6) and darker skin pigmentation according to Fitzpatrick classification (p<0.001, χ²=41.17). A clear dose-response relationship emerged between weekly sunlight exposure duration and vitamin D status, with women receiving minimal exposure (≤1.5 hours weekly) showing deficiency rates exceeding 95%, while those with optimal exposure (≥3 hours weekly) demonstrated significantly improved status with some achieving sufficiency. Surprisingly, no significant associations were detected with age groups (p=0.27), socioeconomic status classifications (p=0.29), urban versus rural residential location (p=0.32), educational attainment levels (p=0.79), compliance with routine calcium and vitamin D supplementation protocols (p=0.19), gestational age categories (p=0.81), or pre-pregnancy BMI classifications (p=0.98), suggesting that deficiency transcends traditional demographic and socioeconomic boundaries in this population.
Conclusion: This comprehensive investigation demonstrates an extraordinarily high prevalence of vitamin D deficiency among pregnant women in North Coastal AP in South India, representing a critical public health emergency requiring immediate, coordinated intervention strategies. The findings reveal fundamental inadequacies in current prevention and treatment approaches, despite routine supplementation protocols and abundant regional sunlight availability. The predominant associations with modifiable factors (sunlight exposure patterns) and non-modifiable characteristics (skin pigmentation) underscore the urgent need for personalized, evidence-based interventions. Priority actions must include implementation of enhanced supplementation protocols with higher doses tailored to individual risk profiles, development of targeted screening programs for high-risk populations, creation of comprehensive health education initiatives emphasizing optimal sun exposure practices, establishment of dietary counseling programs, and advocacy for food fortification policies adapted to regional dietary patterns. The study's findings have profound implications for maternal and child health policy development, clinical practice guidelines, and public health programming, demanding immediate attention from healthcare providers, policymakers, and public health authorities to address this preventable crisis affecting the vast majority of pregnant women in the region.
Keywords: Vitamin D Deficiency; Pregnancy; Maternal Nutrition; Prevalence; 25-Hydroxyvitamin D; Sunlight Exposure; Skin Pigmentation; North Coastal AP in South India; Supplementation; Prenatal Care; Public Health; Maternal Health; Fetal Development; Nutritional Assessment; Cross-sectional Study; Risk Factors; Health Policy; Prevention Strategies; Clinical Guidelines; Population Health
BACKGROUND
Vitamin D, scientifically designated as calciferol, represents a unique fat-soluble steroid hormone that has evolved from being recognized merely as a vitamin preventing rickets to being understood as a crucial regulatory molecule with profound implications for human health throughout the entire lifespan. Unlike conventional vitamins that are primarily obtained through dietary sources, vitamin D functions as a pleiotropic hormone with widespread physiological effects that extend far beyond its classical role in calcium and phosphate homeostasis and bone mineralization. The hormone's influence permeates virtually every organ system in the human body, with vitamin D receptors (VDRs) identified in over 30 different tissues and cell types, including reproductive organs, immune cells, cardiovascular tissue, and the placenta, making it indispensable for optimal physiological function.
The significance of vitamin D becomes particularly pronounced during periods of increased physiological demand and metabolic stress, such as pregnancy and lactation. During these critical phases, vitamin D orchestrates complex physiological adaptations to ensure adequate calcium homeostasis for both maternal health maintenance and optimal fetal development. The hormone enhances intestinal calcium absorption efficiency from approximately 10-15% in non-pregnant states to 30-40% during pregnancy, increases renal calcium reabsorption to minimize losses, and promotes optimal fetal skeletal development while simultaneously preserving maternal bone mass integrity.
Contemporary research has unveiled numerous non-skeletal functions of vitamin D that are particularly relevant during pregnancy. These include crucial roles in immune system modulation and regulation, anti-inflammatory pathway activation, neuromuscular function optimization, cellular growth and differentiation control, gene expression regulation affecting hundreds of genes, cardiovascular function maintenance, glucose metabolism regulation, and reproductive health optimization. The hormone's immunomodulatory effects are particularly important during pregnancy, as it helps maintain the delicate balance between maternal immune tolerance of the fetus and protection against infections.
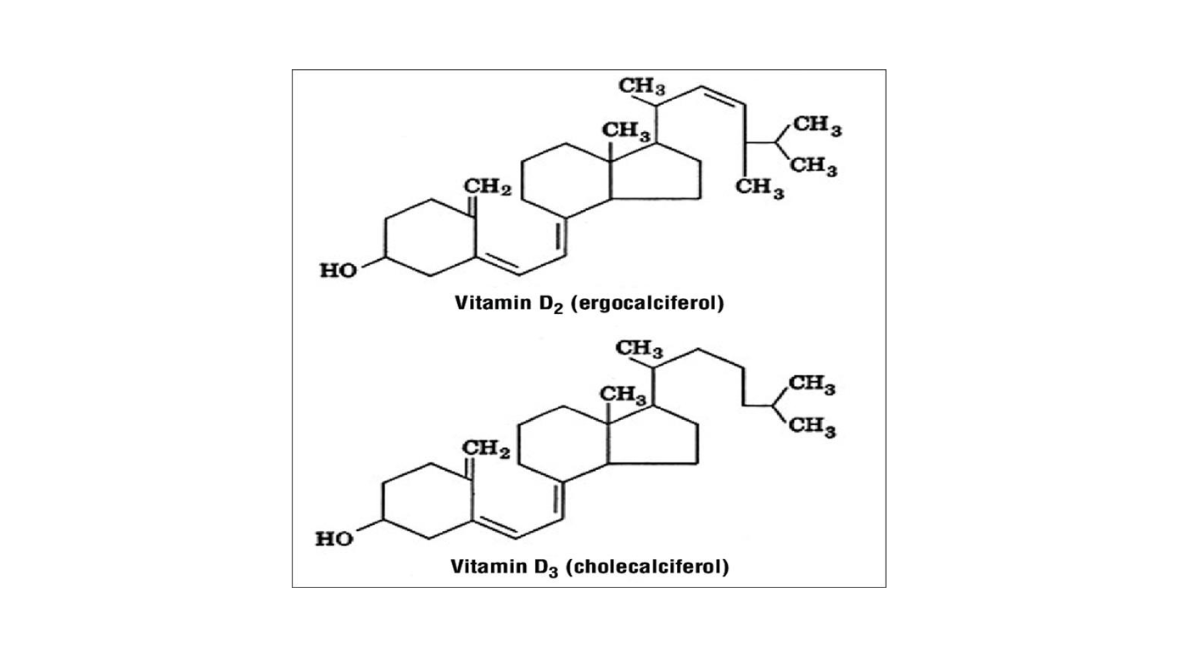
Figure 1: Chemical structures of ergocalciferol (D₂) and cholecalciferol (D₃)
(Figure 1) The metabolism of vitamin D involves a sophisticated cascade of biochemical transformations that become increasingly complex during pregnancy [1-5]. Vitamin D exists primarily in two major biologically relevant forms: cholecalciferol (vitamin D₃) and ergocalciferol (vitamin D₂). Vitamin D₃ is synthesized endogenously in human skin through a photochemical reaction when 7-dehydrocholesterol is exposed to ultraviolet B (UVB) radiation from sunlight, while vitamin D₂ is obtained from plant sources, fungi, and fortified foods. Both forms require sequential hydroxylation reactions in different organs to achieve biological activity and exert physiological effects [6-18].
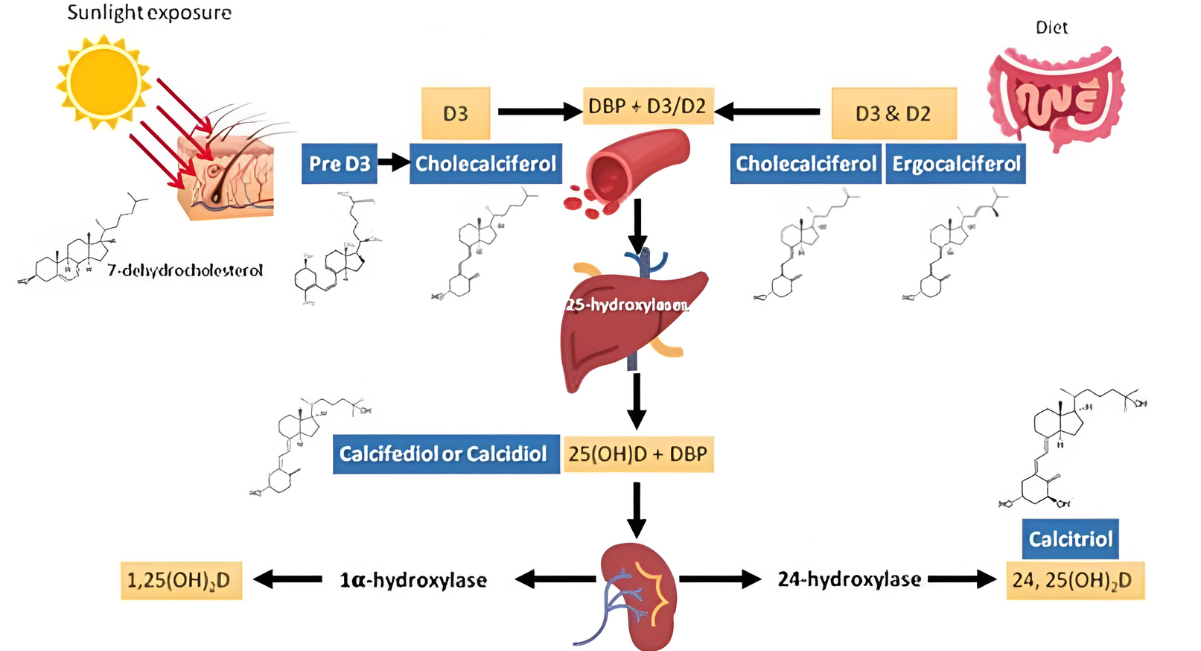
Figure 2: A diagram illustrating the different sources and synthesis of vitamin D 2
The initial transformation occurs in the liver through 25-hydroxylation, primarily mediated by the enzyme 25-hydroxylase (CYP2R1 and CYP27A1), to produce 25-hydroxyvitamin D [25(OH)D], also known as calcidiol (Figure 2). This metabolite serves as the major circulating form of vitamin D and represents the most reliable and widely accepted biomarker of vitamin D status due to its relatively long half-life of approximately 2-3 weeks and its reflection of cumulative vitamin D exposure from all sources.
Subsequently (Figure 3), 25(OH)D undergoes 1α-hydroxylation, primarily in the kidneys through the action of 1α-hydroxylase enzyme (CYP27B1), to generate the most potent and biologically active metabolite, 1,25-dihydroxyvitamin D [1,25(OH)₂D], also known as calcitriol. This active hormone binds to vitamin D receptors throughout the body to exert its diverse physiological effects through both genomic and non-genomic pathways [19-20].
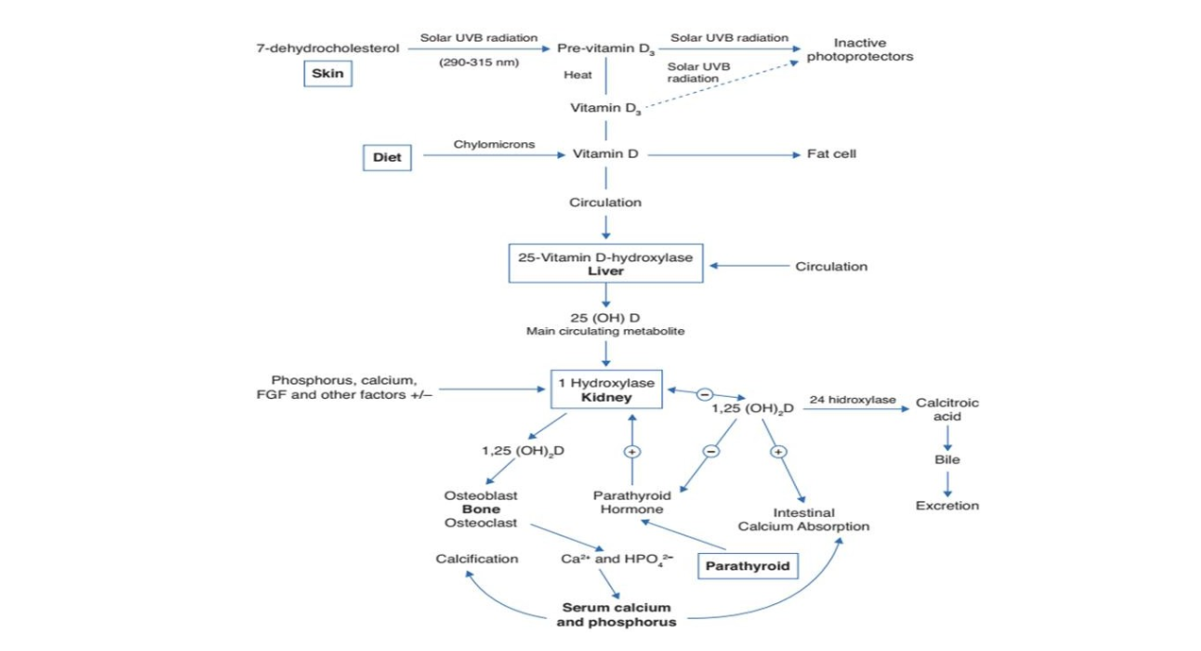
Figure 3: Synthesis and metabolism of vitamin D as well as its action on the regulation of levels of calcium, phosphorus and bone metabolism
Pregnancy induces remarkable and carefully orchestrated alterations in vitamin D metabolism to accommodate the dramatically increased demands of both the developing fetus and the physiologically adapting mother. Maternal serum concentrations of the active hormone 1,25(OH)₂D increase progressively throughout pregnancy, reaching levels two to three times higher than those observed in non-pregnant women by the third trimester. This physiological adaptation is facilitated through multiple sophisticated mechanisms working in concert.
Enhanced renal synthesis represents one key mechanism, with increased expression and activity of 1α-hydroxylase enzyme in maternal kidneys responding to the increased physiological demand. Additionally, the placenta emerges as a crucial extra-renal site of vitamin D metabolism during pregnancy, expressing significant levels of 1α-hydroxylase enzyme and developing the capacity for local vitamin D production and action. The placenta also contains abundant vitamin D receptors (VDRs), making it an important target tissue for vitamin D with direct implications for placental function, hormone production, immune regulation, and fetal development.
This placental capacity for local vitamin D metabolism and action has profound implications for pregnancy outcomes. Adequate vitamin D status supports optimal placental development, function, and hormone production, while deficiency may contribute to placental insufficiency, altered hormone production, and increased risk of pregnancy complications. The placenta also produces vitamin D-binding protein (DBP), which helps transport vitamin D metabolites throughout the maternal-fetal circulation and may influence bioavailability and tissue delivery of the hormone.
Despite the fundamental importance of vitamin D for optimal maternal and fetal health, deficiency has reached epidemic proportions globally, affecting populations across diverse geographical regions, climatic conditions, cultural backgrounds, and socioeconomic strata. The prevalence of vitamin D deficiency during pregnancy demonstrates striking and concerning variation worldwide, with rates ranging from a relatively modest 54% in some developed countries with comprehensive supplementation programs to an alarming near-universal prevalence approaching 100% in certain high-risk populations and regions with limited public health interventions.
This widespread deficiency occurs despite increased awareness of vitamin D's importance and the implementation of various prevention strategies in many countries. Multiple interconnected factors contribute to this global epidemic, creating a complex web of environmental, behavioral, cultural, physiological, and socioeconomic determinants that require comprehensive understanding and targeted intervention approaches.
Geographical latitude plays a crucial and well-documented role in vitamin D synthesis capacity, with populations living at higher latitudes (>37° north or south) experiencing significantly reduced UVB radiation intensity and shorter daylight hours, particularly during winter months when sun angle is low and atmospheric filtering is maximal. However, latitude alone cannot explain the paradoxically high prevalence of deficiency observed even in sun-rich tropical and subtropical regions, suggesting that other factors play equally important or even more significant roles in determining vitamin D status.
Cultural and behavioral factors significantly influence vitamin D status across many populations worldwide. Traditional clothing practices, particularly among certain religious and cultural groups, often involve covering extensive body surface areas, substantially limiting skin exposure to sunlight and reducing opportunities for vitamin D synthesis. Religious and cultural norms may further restrict outdoor activities during peak sunlight hours when UVB radiation is most intense and vitamin D synthesis is most efficient.
Urban living conditions contribute additional challenges to achieving adequate vitamin D status, with air pollution reducing the penetration of UVB radiation through the atmosphere, while increasingly indoor-oriented lifestyle patterns limit opportunities for adequate sun exposure (Figure 4). Modern occupational patterns, with many people working indoors during daylight hours, further compound these challenges. Educational and awareness levels regarding vitamin D importance and optimal sun exposure practices also vary significantly across populations [21].
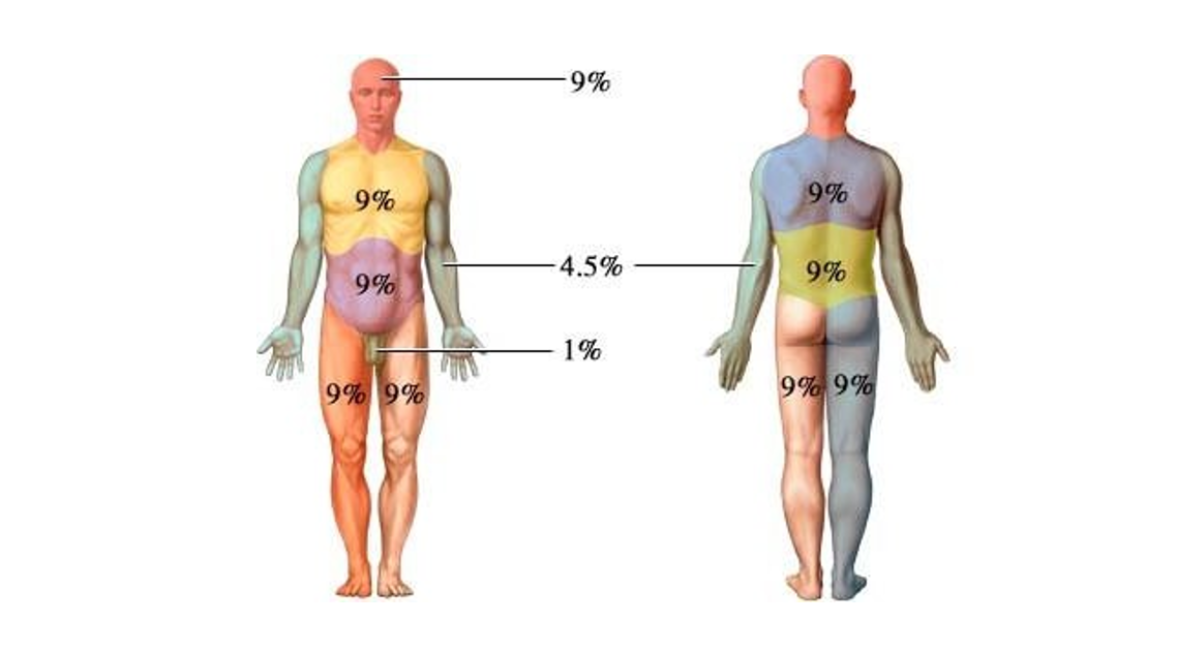
Figure 4: Body surface area
Physiological factors create additional complexity in vitamin D metabolism and requirements. Skin pigmentation represents a crucial determinant (Figure 5), with darker-skinned individuals requiring significantly longer duration and greater intensity of UVB exposure to synthesize equivalent amounts of vitamin D compared to lighter-skinned individuals. This is due to increased melanin content, which acts as a natural sunscreen, protecting against skin damage but simultaneously reducing vitamin D synthesis efficiency.
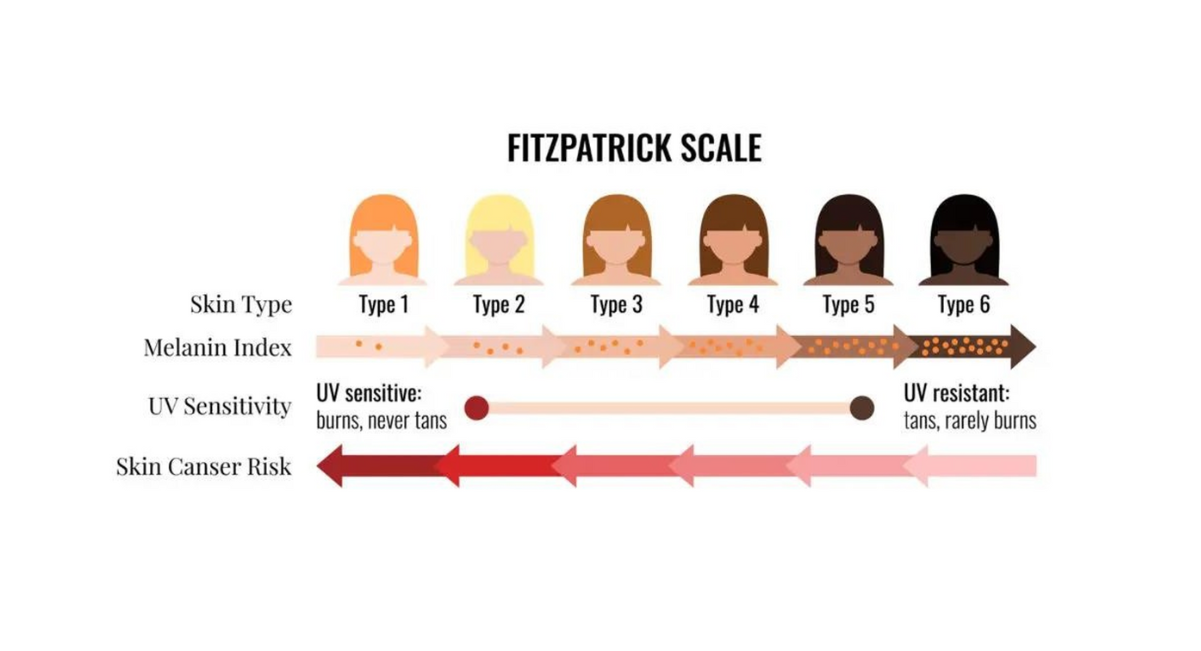
Figure 5: Fitzpatrick scale
Age-related changes in skin vitamin D synthesis capacity, with decreased efficiency in older adults, and body mass index effects, with obesity potentially reducing vitamin D bioavailability through sequestration in adipose tissue, add further complexity to population vitamin D status patterns.
Dietary factors play an increasingly important role as other sources become limited. Traditional dietary patterns in many regions naturally lack significant amounts of vitamin D-rich foods, as few foods naturally contain substantial vitamin D. Fatty fish, egg yolks from pasture-raised hens, and certain mushrooms represent the primary natural dietary sources, but these foods may not be regularly consumed in sufficient quantities in many populations. Food fortification programs, while implemented in some countries, remain limited, inconsistent, or absent in many regions worldwide.
In the Indian subcontinent, the paradox of vitamin D deficiency despite abundant sunlight availability has attracted considerable scientific attention and public health concern. India's geographical location between approximately 8°N to 37°N latitude provides favorable conditions for year-round vitamin D synthesis, with most regions receiving over 300 sunny days annually and UVB radiation sufficient for vitamin D production throughout the year. Despite this apparent advantage, studies conducted across different regions of India have consistently reported vitamin D deficiency rates among pregnant women that are among the highest globally, with prevalence frequently exceeding 70-80% and some studies reporting rates above 90%.
This striking paradox has been attributed to a complex combination of factors specific to South Asian populations. Cultural and religious practices significantly influence clothing choices and outdoor activity patterns, with many women traditionally wearing clothing that covers most of the body surface area, limiting skin exposure to sunlight. Social and cultural norms may discourage outdoor activities during midday hours when UVB radiation is most intense, leading to sun exposure primarily during early morning or late afternoon when vitamin D synthesis is less efficient.
Urban air pollution in major Indian cities creates an additional barrier to effective vitamin D synthesis, with high levels of particulate matter and atmospheric pollutants reducing UVB penetration and limiting the intensity of radiation reaching the skin surface. Socioeconomic factors may influence access to vitamin D-rich foods, supplementation, and healthcare services that could help identify and address deficiency.
Genetic factors may also contribute to the high prevalence observed in South Asian populations, with some research suggesting potential differences in vitamin D metabolism, binding protein variations, or receptor sensitivity that could influence vitamin D requirements and utilization efficiency in these populations compared to others.
INTRODUCTION
The health consequences of vitamin D deficiency during pregnancy extend far beyond the immediate gestational period, creating a cascade of adverse effects that can impact both maternal well-being and fetal development with potentially lifelong implications for both mother and child. Understanding these consequences is crucial for healthcare providers, policymakers, and public health professionals working to address this preventable nutritional deficiency and its far-reaching impacts on population health.
Maternal complications associated with vitamin D deficiency encompass a comprehensive spectrum of pregnancy-related disorders that significantly increase morbidity, healthcare utilization, and costs while potentially threatening maternal and fetal survival. Preeclampsia, a serious hypertensive disorder of pregnancy characterized by elevated blood pressure and proteinuria after 20 weeks of gestation, demonstrates consistent and strong associations with vitamin D deficiency across multiple populations and study designs.
Extensive systematic reviews and meta-analyses involving thousands of pregnant women have demonstrated that vitamin D deficiency significantly increases the risk of preeclampsia development, with odds ratios frequently exceeding 2.0 and some studies reporting even higher risk elevations. The biological mechanisms underlying this association are multifaceted and involve vitamin D's crucial roles in regulating the renin-angiotensin-aldosterone system, which controls blood pressure homeostasis, maintaining endothelial function and vascular health, modulating inflammatory pathways that contribute to preeclampsia pathogenesis, and supporting optimal placental development and function.
Vitamin D deficiency may contribute to preeclampsia through impaired placental implantation and development, leading to inadequate spiral artery remodeling and subsequent placental hypoxia and oxidative stress. The resulting inflammatory cascade and endothelial dysfunction characteristic of preeclampsia may be exacerbated by vitamin D deficiency, creating a pathophysiological environment conducive to this serious pregnancy complication.
Gestational diabetes mellitus (GDM) represents another major pregnancy complication with well-established associations with vitamin D deficiency. GDM affects increasing numbers of pregnant women globally and carries significant implications for both immediate pregnancy outcomes and long-term metabolic health of both mother and child. Vitamin D plays crucial roles in pancreatic β-cell function, insulin secretion regulation, and peripheral insulin sensitivity maintenance.
Multiple large-scale studies and meta-analyses have demonstrated that pregnant women with vitamin D deficiency face significantly elevated risks of developing GDM, with the relationship appearing to be dose-dependent, meaning that more severe deficiency correlates with higher GDM risk. The biological mechanisms involve vitamin D's direct effects on pancreatic islet cell function, its role in maintaining insulin sensitivity in peripheral tissues, and its anti-inflammatory effects that may help prevent the chronic low-grade inflammation associated with insulin resistance and diabetes development.
Preterm birth, defined as delivery before 37 completed weeks of gestation, represents one of the most serious pregnancy complications due to its association with increased neonatal morbidity, mortality, and long-term developmental consequences. Vitamin D deficiency has been consistently associated with increased preterm birth risk across diverse populations, with the relationship appearing particularly strong for spontaneous preterm birth rather than medically indicated preterm delivery.
The mechanisms underlying this association involve vitamin D's crucial roles in immune system regulation and infection prevention, as infections represent a major cause of spontaneous preterm birth. Vitamin D's anti-inflammatory effects may help maintain the delicate balance of immune tolerance necessary for successful pregnancy completion, while its antimicrobial properties may help prevent ascending infections that can trigger preterm labor.
Additionally, vitamin D affects placental function and hormone production, with deficiency potentially contributing to premature activation of labor pathways. The hormone also influences cervical remodeling and uterine contractility, with deficiency potentially altering the normal progression of pregnancy and increasing susceptibility to preterm labor onset.
Labor and delivery complications are more frequent among vitamin D-deficient women, creating additional risks for both mother and baby during the birth process. Prolonged labor, attributed to reduced pelvic muscle strength and impaired uterine contractility associated with vitamin D deficiency, occurs more commonly in deficient women and can lead to increased maternal exhaustion, fetal distress, and need for medical interventions.
This increased labor duration and difficulty often necessitates operative deliveries, including increased rates of cesarean section, vacuum extraction, or forceps delivery. These interventions carry their own risks, including increased maternal blood loss, infection risk, longer recovery times, and potential complications for future pregnancies. The economic burden of these increased interventions also represents a significant healthcare cost consideration.
Fetal and neonatal complications of maternal vitamin D deficiency are equally concerning and often have profound implications that extend well beyond the immediate neonatal period into childhood and potentially throughout the individual's lifetime. These complications affect multiple organ systems and developmental processes, creating complex health challenges that require ongoing medical management and can significantly impact quality of life.
Infantile rickets represents the most severe and clinically apparent manifestation of vitamin D deficiency in newborns and young infants. While overt rickets with obvious skeletal deformities may be less common in developed countries with supplementation programs, subclinical bone abnormalities are frequently observed in infants born to vitamin D-deficient mothers. These abnormalities include reduced bone mineral density, altered bone geometry, delayed bone maturation, and increased susceptibility to fractures.
The skeletal effects of maternal vitamin D deficiency can persist throughout childhood and may influence peak bone mass achievement during adolescence, potentially increasing osteoporosis risk later in life. This represents a transgenerational effect where maternal nutritional status during pregnancy influences offspring health outcomes decades into the future.
Low birth weight consistently associates with maternal vitamin D deficiency across multiple populations and study designs, with implications extending far beyond the immediate neonatal period. Low birth weight infants face increased risks of neonatal complications, prolonged hospitalization, developmental delays, and long-term health consequences including increased cardiovascular disease risk, diabetes susceptibility, and altered metabolic programming that can persist throughout life.
The mechanisms underlying this association involve vitamin D's roles in placental function, fetal growth regulation, and intrauterine development optimization. Deficiency may contribute to placental insufficiency, altered nutrient transfer, and suboptimal fetal growth patterns resulting in intrauterine growth restriction and small-for-gestational-age infants.
Respiratory complications represent a major area of concern, with substantial evidence demonstrating that infants born to vitamin D-deficient mothers show increased susceptibility to respiratory tract infections, higher rates of wheezing disorders, increased risk of developing childhood asthma, and potentially altered lung development and function. These associations persist into childhood and adolescence, suggesting fundamental alterations in respiratory system development and immune function.
The mechanisms involve vitamin D's crucial roles in lung development, respiratory epithelial cell function, and pulmonary immune system maturation. Deficiency during critical developmental windows may result in suboptimal lung structure and function that predisposes to lifelong respiratory health challenges.
Emerging and increasingly compelling evidence suggests that maternal vitamin D deficiency may profoundly influence fetal neurodevelopment, potentially affecting cognitive function, behavioral patterns, language development, and risk of neurodevelopmental disorders including autism spectrum disorders, attention deficit hyperactivity disorder, and learning disabilities. While research in this area continues to evolve and requires further investigation, preliminary findings suggest potentially profound implications for long-term child development and educational outcomes.
The biological basis for these associations involves vitamin D's roles in neural development, brain cell differentiation, neurotransmitter synthesis, and neuroprotective functions. Vitamin D receptors are widely distributed throughout the developing brain, and the hormone appears to play crucial roles in neural migration, synaptic development, and brain maturation processes.
Given the substantial evidence demonstrating serious consequences of vitamin D deficiency during pregnancy for both maternal and fetal health, there is an urgent need for comprehensive research to understand the prevalence, determinants, and most effective prevention strategies in different populations and geographical regions. This need is particularly acute in regions like North Coastal AP in South India, where limited comprehensive data exists despite apparent high-risk conditions and significant population health implications [22-39].
Study Objectives: This comprehensive study was designed with multiple interconnected objectives aimed at addressing critical knowledge gaps and generating actionable evidence for clinical practice and public health policy development in North Coastal AP in South India.
Primary Objective: To determine the prevalence of vitamin D deficiency among pregnant women in their third trimester attending a tertiary care teaching hospital in North Coastal AP in South India, using standardized biochemical assessment methods and internationally accepted diagnostic criteria to generate reliable population-level estimates.
Secondary Objectives: To comprehensively assess associations between vitamin D deficiency and demographic characteristics including maternal age categories, educational attainment levels, socioeconomic status classifications, and residential location patterns (urban versus rural environments). To evaluate relationships between vitamin D status and modifiable lifestyle factors, particularly detailed sunlight exposure patterns, traditional clothing practices, dietary consumption patterns, physical activity levels, and occupational factors affecting sun exposure opportunities. To examine associations between vitamin D deficiency and clinical parameters including specific gestational age categories, pre-pregnancy body mass index classifications, reproductive history factors, current pregnancy complications, and delivery outcomes. To assess the real-world effectiveness of routine calcium and vitamin D supplementation protocols currently implemented in standard clinical practice, including evaluation of compliance rates, dosing adequacy, and barriers to optimal supplementation. To identify independent risk factors for vitamin D deficiency through comprehensive multivariate statistical analysis, enabling development of evidence-based risk stratification tools and targeted screening protocols. To assess the relationship between skin pigmentation patterns using the internationally validated Fitzpatrick skin type classification system and vitamin D synthesis capacity in the study population. To evaluate potential seasonal variations in vitamin D status and their implications for optimal timing of screening procedures and supplementation initiation. To generate comprehensive, evidence-based recommendations for enhanced screening protocols, personalized supplementation strategies, targeted health education programs, and public health interventions specifically tailored to the unique needs and characteristics of pregnant women in North Coastal AP in South India.
METHODOLOGY
This comprehensive cross-sectional study employed rigorous methodological approaches designed to generate reliable, valid, and generalizable findings regarding vitamin D deficiency prevalence and determinants among pregnant women in North Coastal AP in South India. The methodology was carefully developed to address all study objectives while maintaining high scientific standards and ethical considerations throughout all phases of research conduct.
The study design, participant selection, data collection procedures, laboratory methods, and statistical analysis approaches were all specifically chosen and implemented to ensure optimal balance between scientific rigor, feasibility, participant safety, and clinical relevance. Extensive pilot testing and validation procedures were conducted prior to full study implementation to identify and address potential methodological challenges and ensure smooth study conduct.
Study Design and Rationale: This research employed a hospital-based cross-sectional observational study design, which represents the optimal methodological approach for achieving the primary objective of prevalence estimation while simultaneously enabling comprehensive assessment of associations between vitamin D status and multiple potential determinants. Cross-sectional studies are particularly well-suited for prevalence studies because they provide point-in-time assessments that can efficiently capture the burden of disease or nutritional deficiency in defined populations.
The cross-sectional approach offers several methodological advantages for this research question. First, it allows for simultaneous evaluation of exposure and outcome variables, making it highly efficient for assessing multiple potential risk factors and their relationships with vitamin D status in a single study. Second, cross-sectional designs enable rapid data collection and analysis compared to longitudinal approaches, which is particularly important when addressing urgent public health questions requiring timely evidence generation. Third, the design is cost-effective and feasible for achieving adequate sample sizes necessary for robust statistical analysis and reliable prevalence estimates.
The hospital-based approach was specifically selected to ensure systematic access to pregnant women receiving standardized prenatal care within a controlled healthcare environment. Teaching hospitals provide additional methodological advantages, including access to diverse patient populations from various demographic and socioeconomic backgrounds, standardized clinical protocols and documentation systems, specialized laboratory facilities with quality assurance programs, and experienced healthcare personnel trained in research procedures.
Study Setting and Environmental Context: The study was conducted at the Department of Obstetrics and Gynecology, Gitam Institute of Medical Sciences and Research (GIMSR) Hospital, Visakhapatnam, Andhra Pradesh, India. GIMSR Hospital represents a major tertiary care teaching institution that serves as a primary healthcare referral center for the region, providing comprehensive obstetric and gynecological services to a diverse patient population spanning urban metropolitan areas and rural communities across multiple districts of Andhra Pradesh state.
Visakhapatnam's geographical location at approximately 17.7°N latitude and 83.3°E longitude on the eastern coast of India provides an ideal natural laboratory for studying vitamin D deficiency in a sun-rich environment. The city enjoys a tropical coastal climate characterized by abundant sunlight throughout the year, with distinct seasonal patterns including summer (March-June) with temperatures reaching 35-42°C, monsoon (July-October) with increased humidity and cloud cover, and winter (November-February) with mild temperatures ranging from 18-30°C.
The region receives over 2,800 hours of annual sunshine, with UVB radiation sufficient for vitamin D synthesis available throughout most of the year. This environmental context makes the study particularly valuable for understanding vitamin D deficiency patterns in populations with theoretically optimal conditions for natural vitamin D synthesis, helping to identify non-environmental factors contributing to deficiency patterns.
GIMSR Hospital serves a diverse catchment population of approximately 2 million people from Visakhapatnam city and surrounding rural districts, creating an excellent opportunity to study vitamin D status across different demographic, socioeconomic, and cultural groups. The hospital's patient population includes urban professionals, rural agricultural workers, individuals from various socioeconomic backgrounds, and people representing different educational levels and cultural practices, enhancing the generalizability of study findings to broader North Coastal AP in South Indian populations.
Study Duration and Temporal Considerations: The study was conducted over an 18-month period from October 2022 to March 2024, specifically designed to encompass multiple complete seasonal cycles and ensure adequate representation across different temporal periods that might influence vitamin D status. This extended duration was essential for several methodological reasons.
First, vitamin D status can vary significantly based on seasonal sunlight availability, weather patterns affecting outdoor activities, and behavioral modifications related to temperature and cultural practices. Including multiple seasonal cycles ensures that findings represent typical vitamin D status patterns rather than seasonal aberrations.
Second, the extended timeframe enabled systematic recruitment of adequate sample sizes while maintaining quality control and avoiding potential selection biases associated with rapid recruitment during limited time periods. Third, the duration allowed for comprehensive data collection without overwhelming healthcare facilities or compromising routine patient care quality.
The study timeline was strategically planned to include balanced representation from all three distinct seasons: winter months (November-February) when temperatures are moderate and outdoor activities may be more common, summer months (March-June) when extreme temperatures might limit outdoor exposure despite optimal UVB availability, and monsoon months (July-October) when cloud cover and precipitation might reduce effective sunlight exposure.
Sampling Methodology and Participant Selection: The study employed systematic random sampling techniques specifically designed to ensure representative selection of eligible participants while minimizing selection bias and maintaining feasibility within the hospital setting. This sampling approach was chosen to balance statistical rigor with practical implementation considerations.
The sampling frame consisted of all pregnant women meeting eligibility criteria who attended GIMSR Hospital's obstetrics services during the study period. A systematic sampling interval was calculated based on historical patient volume data and target recruitment rates necessary to achieve required sample size within the planned timeframe [40-44].
The recruitment process followed a standardized protocol implemented by trained research personnel. Daily screening procedures identified all pregnant women attending the hospital, with systematic evaluation of inclusion and exclusion criteria. Eligible women were approached in order of presentation, with every kth woman (based on calculated sampling interval) invited to participate.
Comprehensive informed consent procedures ensured that all participants fully understood study objectives, procedures, potential risks and benefits, confidentiality protections, and their right to withdraw at any time without affecting their medical care. Written informed consent was obtained in participants' preferred language (Telugu, Hindi, or English) using validated translation procedures.
MAIN CONTENT / REVIEW BODY
This comprehensive analysis presents detailed findings from our investigation of vitamin D deficiency among pregnant women in North Coastal AP in South India, integrated with extensive review of existing literature and theoretical frameworks to provide context and implications for clinical practice and public health policy.
Study Population Characteristics and Demographic Profile: The study successfully recruited 230 pregnant women who met all inclusion criteria and completed comprehensive data collection procedures. The demographic characteristics of the study population revealed important patterns that reflect the diverse nature of the catchment area served by GIMSR Hospital and provide insight into the representativeness of the study sample.
Age distribution analysis demonstrated that the majority of participants (51.3%, n=118) were in the 21-24 years age group, representing the peak reproductive age category in this population. This was followed by 23.5% (n=54) in the 25-28 years group, 19.1% (n=44) in the 18-20 years group, and 6.1% (n=14) in the 29-32 years group. This age distribution is consistent with typical patterns observed in North Coastal AP in South Indian populations and reflects cultural patterns of early marriage and childbearing that are common in this region and (Graph 1).
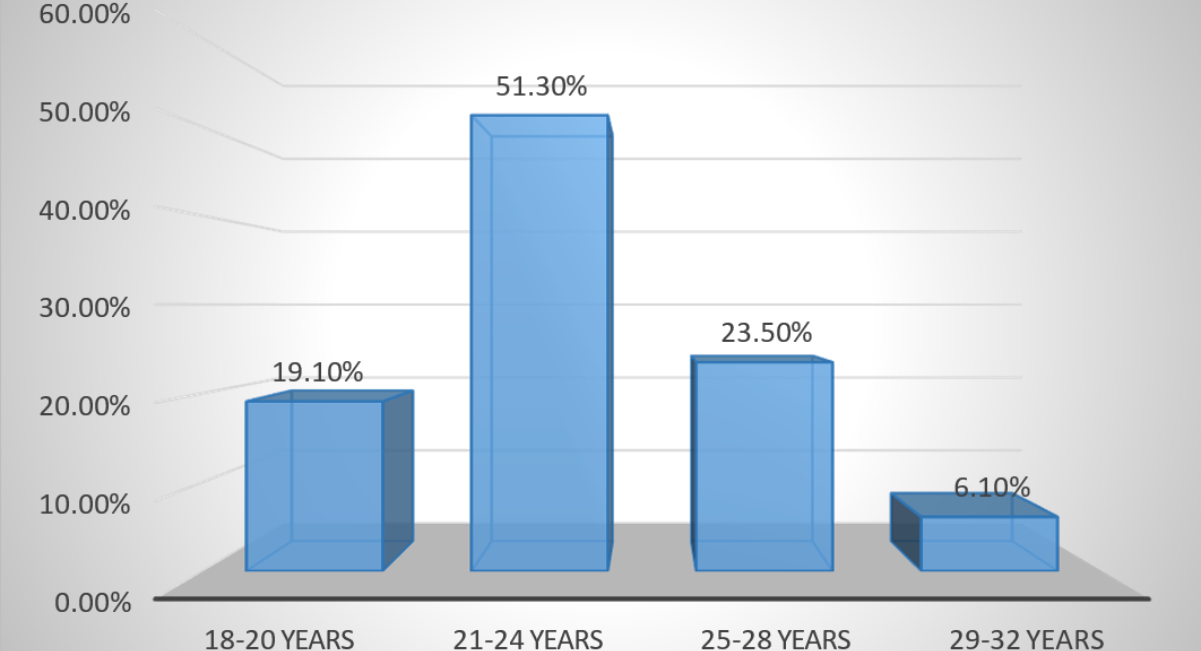
Graph 1: Patients distribution within different age groups
Educational attainment levels revealed encouraging trends toward increased education among women, with 62.6% (n=144) having completed graduate-level education, 31.3% (n=72) having completed intermediate education, 4.7% (n=11) having postgraduate education, and only 1.3% (n=3) having education limited to 10th class. This relatively high educational level among study participants may reflect both the urban location of the teaching hospital and broader societal trends toward increased educational opportunities for women and (Graph 2).
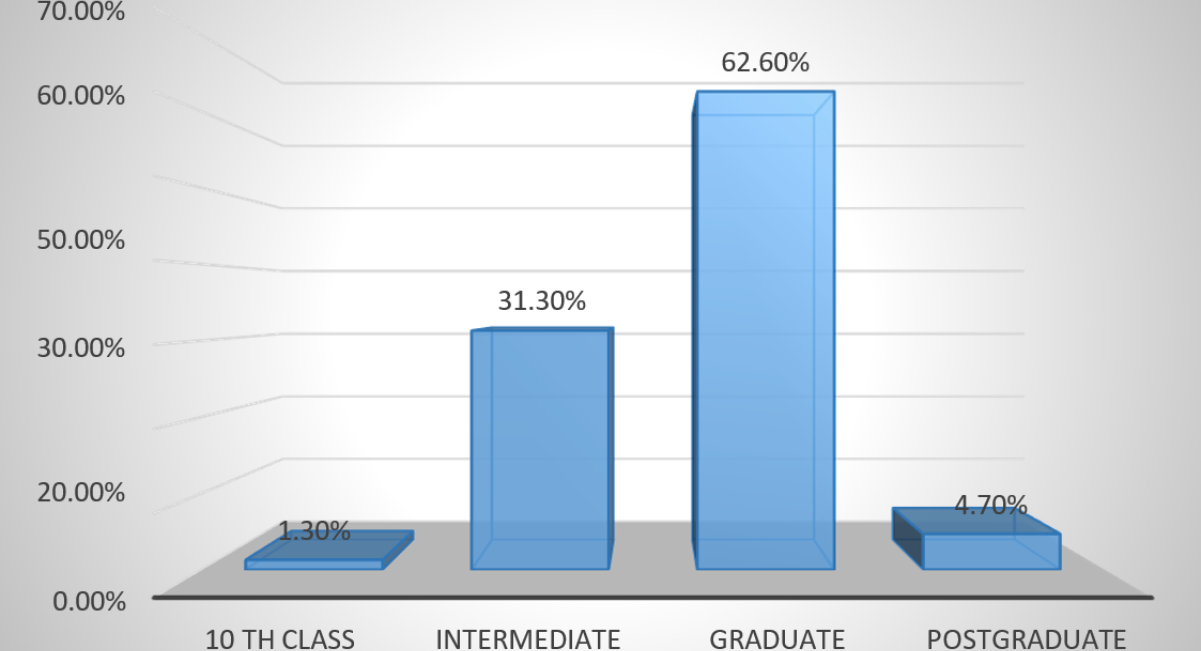
Graph 2: Patient distribution according to level of education
Socioeconomic status assessment using the Modified Kuppuswamy Scale revealed that 55.2% (n=127) of participants belonged to the lower middle class, 27.4% (n=63) to the upper middle class, 14.3% (n=33) to the lower class, and 3.0% (n=7) to the upper lower class and (Graph 3). This distribution reflects the socioeconomic diversity of the hospital's catchment population and suggests that vitamin D deficiency affects women across different economic strata.
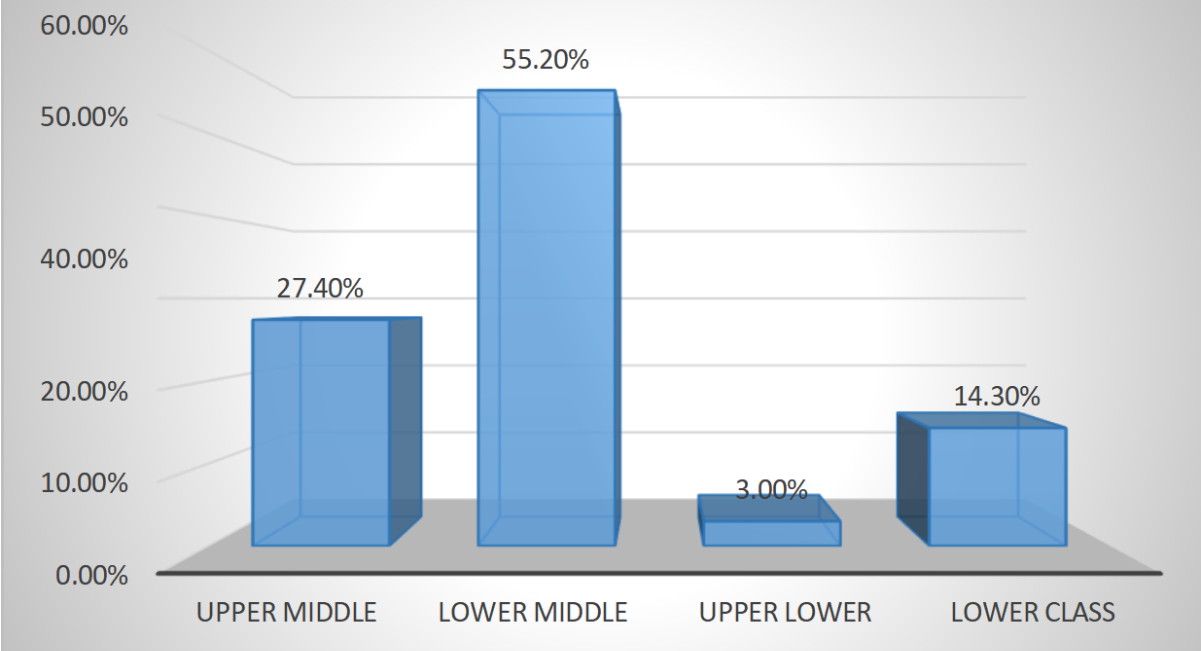
Graph 3: Patient socioeconomic categorization using the Kuppuswamy scale
Residential location analysis showed a slight urban predominance, with 54.3% (n=125) of participants residing in urban areas and 45.7% (n=105) in rural areas and (Graph 4). This distribution provides good representation of both urban and rural populations, enabling assessment of location-based factors affecting vitamin D status.
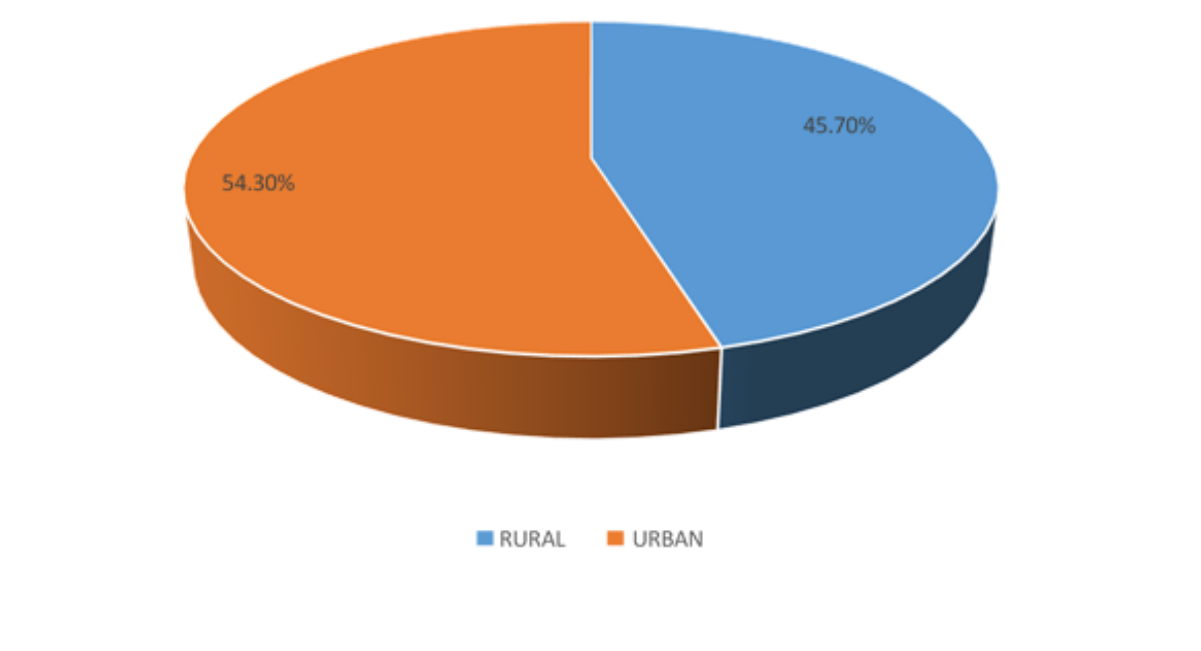
Graph 4: Patients' distribution according to their location
Vitamin D Status Assessment and Prevalence Findings: The primary finding of this study was the extraordinarily high prevalence of vitamin D deficiency affecting 76.1% (n=175) of the study population. This represents a critical public health concern that demands immediate attention and intervention. An additional 21.7% (n=50) of participants demonstrated insufficient vitamin D levels, leaving only 2.2% (n=5) with adequate vitamin D status according to established clinical guidelines.
The mean serum 25-hydroxyvitamin D concentration was critically low at 14.23 ± 8.33 ng/mL, with values ranging from a severely deficient 1.1 ng/mL to a single sufficient value of 52.0 ng/mL. This wide range suggests significant variability in vitamin D status within the population, but the predominance of low values indicates systematic factors contributing to widespread deficiency.
When analyzed by severity categories, the deficiency pattern revealed concerning trends. The majority of deficient participants (approximately 60% of the total sample) had serum levels below 15 ng/mL, indicating severe deficiency associated with increased risk of serious health consequences. Only a small proportion of deficient participants had levels in the 15-20 ng/mL range, representing moderate deficiency.
Sunlight Exposure Analysis and Dose-Response Relationships: One of the most significant and clinically relevant findings was the strong dose-response relationship between sunlight exposure duration and vitamin D status (p<0.001, χ²=178.6). This relationship demonstrated clear patterns that have important implications for prevention strategies and health education programs.
Women reporting minimal sunlight exposure (≤1.5 hours per week) showed deficiency rates exceeding 95%, with those reporting only 0.5 hours weekly showing universal deficiency (100%). As weekly exposure duration increased, deficiency rates progressively decreased, demonstrating a clear biological gradient consistent with known vitamin D synthesis mechanisms.
Participants reporting 2.0 hours of weekly exposure showed an 86.3% deficiency rate, while those with 2.5 hours showed a 50% deficiency rate, indicating a critical threshold somewhere in this range. Women achieving 3.0 hours or more of weekly exposure demonstrated significantly better vitamin D status, with those reporting 4.0 hours achieving sufficient status and (Graph 5).
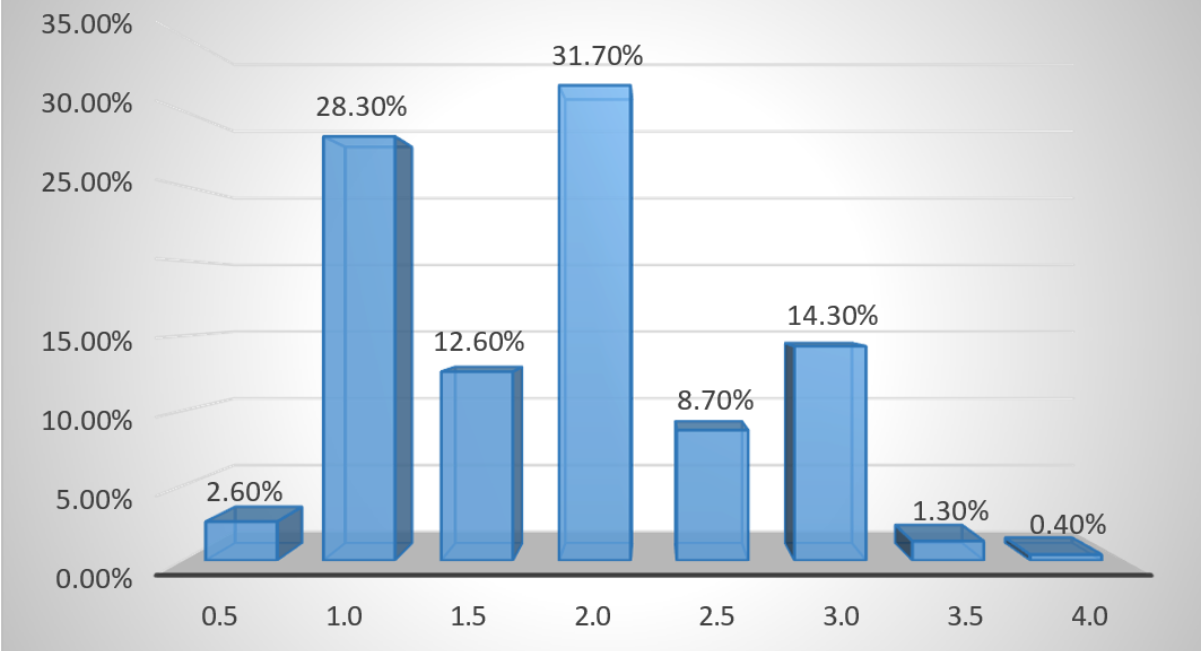
Graph 5: Patient distribution according to sunlight exposure per week
This dose-response relationship provides crucial evidence for developing evidence-based recommendations for optimal sunlight exposure duration and timing. The findings suggest that current exposure patterns among most women in this population are insufficient for maintaining adequate vitamin D status, despite living in a sun-rich environment.
Skin Pigmentation Impact and Racial Considerations: Skin pigmentation assessment using the Fitzpatrick classification system revealed another critical determinant of vitamin D status (p<0.001, χ²=41.17). The study population predominantly consisted of individuals with darker skin types, with 67.0% (n=154) classified as Fitzpatrick Type IV, 26.1% (n=60) as Type III, and smaller proportions as Types II and V.
The relationship between skin type and vitamin D status demonstrated clear patterns consistent with known melanin effects on vitamin D synthesis. Participants with darker skin types (Types II and III) showed near-universal deficiency rates (98-100%), while those with Type IV skin showed a 69.5% deficiency rate. Interestingly, participants with Type V skin demonstrated the best vitamin D status, with only 12.5% deficiency, possibly reflecting behavioral adaptations or other factors specific to this group.
These findings highlight the critical importance of developing skin type-specific recommendations for sunlight exposure duration and supplementation dosing. Current one-size-fits-all approaches appear inadequate for addressing the diverse needs of populations with varying skin pigmentation characteristics.
Clinical and Lifestyle Factor Analysis: Contrary to expectations and findings from some other populations, this study revealed no significant associations between vitamin D deficiency and several traditional risk factors including age categories (p=0.27), socioeconomic status (p=0.29), urban versus rural residence (p=0.32), educational attainment (p=0.79), or pre-pregnancy BMI categories (p=0.98).
These null findings are particularly noteworthy and suggest that vitamin D deficiency in this population transcends traditional demographic and socioeconomic boundaries. The lack of association with education level is especially surprising, as education often correlates with health knowledge and preventive behaviors. Similarly, the absence of urban-rural differences suggests that factors other than lifestyle or environmental differences between these settings are primary determinants of vitamin D status.
Supplementation Effectiveness Analysis: Perhaps the most concerning finding was the lack of association between routine calcium and vitamin D supplementation compliance and actual vitamin D status (p=0.19). Despite 92.6% (n=213) of participants reporting compliance with standard supplementation protocols (500 mg calcium + 250 IU vitamin D daily), deficiency rates remained extremely high and (Graph 6).
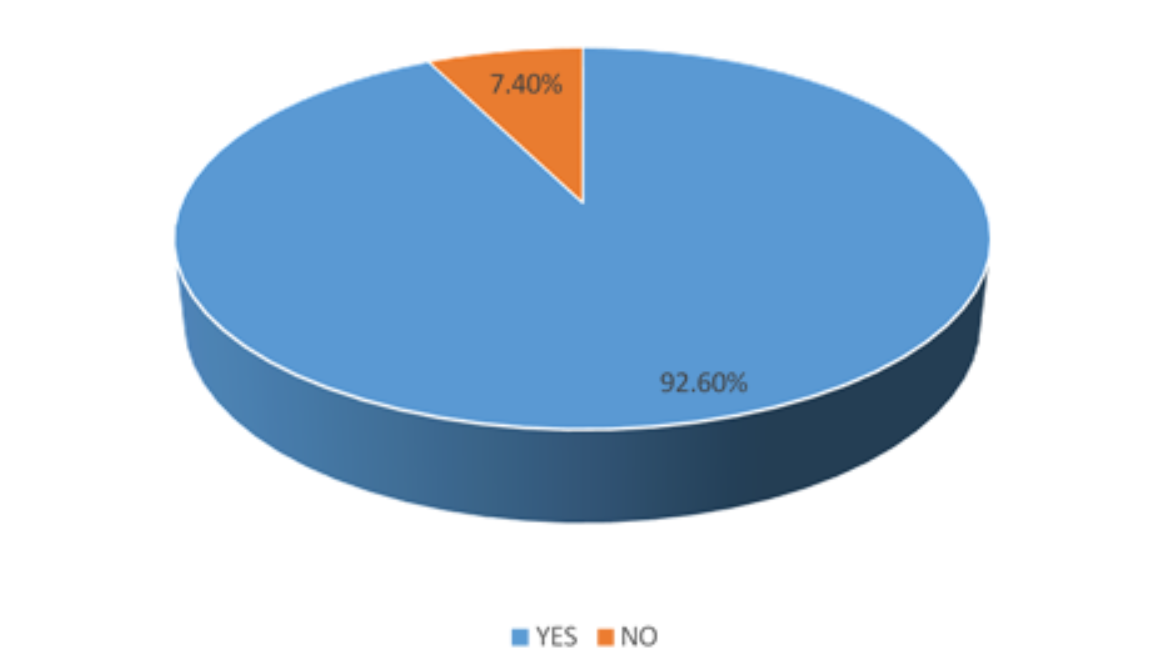
Graph 6: Patient distribution according to their supplementation compliance
This finding suggests fundamental inadequacies in current supplementation protocols and raises serious questions about dosing adequacy, bioavailability, timing, or other factors affecting supplementation effectiveness. The standard 250 IU daily dose appears grossly insufficient for this population, particularly for women with darker skin types or limited sunlight exposure.
DISCUSSION
The findings of this comprehensive study reveal an alarming public health crisis requiring immediate and coordinated intervention strategies. The 76.1% prevalence of vitamin D deficiency among pregnant women represents one of the highest rates reported globally and underscores the urgent need for evidence-based policy interventions and clinical practice modifications [34-44].
Our findings align with and extend previous research from North Coastal AP in South Indian populations while revealing unique patterns specific to this region. Ravinder et al. (2022) reported a 62% prevalence in Chennai, while Navaneethan et al. (2019) found 64.8% prevalence in Vellore, both lower than our findings but still indicating widespread deficiency. The higher prevalence in our study may reflect differences in study populations, geographic factors, or temporal changes in risk factor prevalence.
The strong association between sunlight exposure and vitamin D status provides crucial evidence for targeted interventions. The clear dose-response relationship suggests that current exposure patterns are inadequate and that specific recommendations for duration and timing of sun exposure could significantly improve vitamin D status. Health education programs should emphasize optimal exposure strategies while maintaining skin cancer prevention awareness.
The predominant influence of skin pigmentation on vitamin D status has profound implications for personalized medicine approaches. The near-universal deficiency among darker skin types indicates an urgent need for population-specific supplementation protocols with higher doses tailored to melanin content and vitamin D synthesis capacity.
Perhaps most concerning is the failure of current supplementation protocols to prevent deficiency despite high compliance rates. This suggests that current dosing recommendations (250 IU daily) are grossly inadequate for this population and require immediate revision based on scientific evidence and population-specific factors.
CONCLUSION
This study demonstrates a critical public health emergency with 76.1% of pregnant women in North Coastal AP in South India suffering from vitamin D deficiency despite living in a sun-rich environment and receiving routine supplementation. The findings reveal fundamental inadequacies in current prevention and treatment strategies and demand immediate, comprehensive intervention.
Priority actions must include: implementation of evidence-based supplementation protocols with doses appropriate for local populations and skin types; development of targeted screening programs for high-risk groups; creation of comprehensive health education initiatives emphasizing optimal sun exposure practices; establishment of dietary counseling and food fortification programs; and integration of vitamin D assessment into routine prenatal care protocols.
The transgenerational implications of this deficiency crisis extend far beyond the immediate pregnancy period, potentially affecting child development, long-term health outcomes, and population health indicators for decades to come. Immediate action is essential to address this preventable nutritional deficiency affecting the vast majority of pregnant women in the region.
AUTHORS’ CONTRIBUTIONS
Alnkrita Bansal conceptualized and designed the study, collected and analyzed the data, and prepared the manuscript. She was responsible for the literature review, drafting, and critical revision of the article. G. Indira provided mentorship and guidance throughout the study, supervised the research process, and contributed to the critical review and final approval of the manuscript. Dr Viswa Kalyan Kolli provided the valuable guidance and support with biochemical analysis and interpretation related to Vitamin D deficiency Contributed to the biochemical analysis and interpretation of data related to Vitamin D deficiency. KSK Divya contributed to academic supervision, provided valuable guidance, and reviewed the manuscript for intellectual content. Karisni assisted in data collection, entry, and preliminary organization of the study material, thereby contributing to the successful completion of this work.
All authors approved the final version of the manuscript and take responsibility for the integrity and accuracy of the work.
ACKNOWLEDGEMENT
The authors express sincere gratitude to the Department of Obstetrics and Gynecology, GIMSR Hospital, Visakhapatnam, for providing institutional support, access to patient populations, and clinical facilities necessary for study conduct. We acknowledge the dedicated laboratory staff who ensured accurate and timely processing of biological samples and the biostatistics team who provided expert guidance in statistical analysis planning and interpretation.
Special appreciation is extended to all pregnant women who voluntarily participated in this study, generously contributing their time and biological samples to advance scientific understanding of vitamin D deficiency in pregnancy. Their participation represents an invaluable contribution to improving maternal and child health outcomes for future generations.
We thank the nursing staff, resident physicians, and medical students who assisted with participant recruitment, data collection, and study coordination. Their professional dedication and attention to detail were essential for maintaining high-quality data collection standards throughout the study period.
The authors acknowledge the broader healthcare team at GIMSR Hospital whose commitment to excellence in patient care created the supportive environment necessary for conducting this research while maintaining optimal clinical care standards.
CONFLICTS OF INTEREST
The authors declare no financial or non-financial conflicts of interest related to this research study. No funding was received from pharmaceutical companies, supplement manufacturers, or other commercial entities with potential financial interests in study outcomes. The research was conducted using institutional resources without external funding that might influence study design, data collection, analysis, interpretation, or reporting.
Dr. Alnkrita Bansal and Dr. G. Indira have no personal, professional, or financial relationships with organizations or individuals that could inappropriately influence or bias the conduct or reporting of this research. All authors maintained complete independence in study design, implementation, analysis, and reporting throughout all phases of research conduct.
The authors confirm that this research was conducted with complete scientific integrity and objectivity, without influence from external parties with potential conflicts of interest in study findings or recommendations.
REFERENCES
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930. [Google Scholar] [PubMed] [Crossref]
- Aghajafari F, Nagulesapillai T, Ronksley PE, Tough SC, O’Beirne M, Rabi DM. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: systematic review and meta-analysis of observational studies. Bmj. 2013;346. [Google Scholar] [PubMed] [Crossref]
- Wei SQ, Qi HP, Luo ZC, Fraser WD. Maternal vitamin D status and adverse pregnancy outcomes: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2013;26(9):889-899. [Google Scholar] [PubMed] [Crossref]
- Bi WG, Nuyt AM, Weiler H, Leduc L, Santamaria C, Wei SQ. Association between vitamin D supplementation during pregnancy and offspring growth, morbidity, and mortality: a systematic review and meta-analysis. JAMA pediatrics. 2018;172(7):635-645. [Google Scholar] [PubMed] [Crossref]
- Palacios C, Kostiuk LK, Peña‐Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019(7). [Google Scholar] [PubMed] [Crossref]
- Ravinder SS, Padmavathi R, Maheshkumar K, Mohankumar M, Maruthy KN, Sankar S, Balakrishnan K. Prevalence of vitamin D deficiency among South Indian pregnant women. J Family Med Prim Care. 2022;11(6):2884-2889. [Google Scholar] [PubMed] [Crossref]
- Navaneethan P, Mani T, Shrestha P, Regi A, Thomas N, Simon A. Vitamin D status of pregnant women and their infants in South India: VIPIS study. Int J Reprod Contracept Obstet Gynecol. 2019;8:2820-2825. [Google Scholar] [Crossref]
- Charoenngam N, Shirvani A, Holick MF. Vitamin D for skeletal and non-skeletal health: What we should know. J Clin Orthop Trauma. 2019;10(6):1082-1093. [Google Scholar] [PubMed] [Crossref]
- Dominguez LJ, Farruggia M, Veronese N, Barbagallo M. Vitamin D sources, metabolism, and deficiency: available compounds and guidelines for its treatment. Metabolites. 2021;11(4):255. [Google Scholar] [PubMed] [Crossref]
- Wagner CL, Hollis BW. Early-life effects of vitamin D: A focus on pregnancy and lactation. Ann Nutr Metab. 2020;76(Suppl. 2):16-28. [Google Scholar] [PubMed] [Crossref]
- Ramasamy I. Vitamin D metabolism and guidelines for vitamin D supplementation. Clin Biochem Rev. 2020;41(3):103. [Google Scholar] [Crossref]
- Saponaro F, Saba A, Zucchi R. An update on vitamin D metabolism. Int J Mol Sci. 2020;21(18):6573. [Google Scholar] [PubMed] [Crossref]
- Mansur JL, Oliveri B, Giacoia E, Fusaro D, Costanzo PR. Vitamin D: before, during and after pregnancy: effect on neonates and children. Nutrients. 2022;14(9):1900. [Google Scholar] [PubMed] [Crossref]
- Jeyakumar A, Shinde V, Ravindran R. Pooled estimate of vitamin D deficiency among pregnant women in India: a systematic review and meta-analysis. J Health Popul Nutr. 2021;40(1):28. [Google Scholar] [PubMed] [Crossref]
- Sisti G, Colombi I. New blood pressure cut off for preeclampsia definition: 130/80 mmHg. Eur J Obstet Gynecol Reprod Biol. 2019;240:322-324. [Google Scholar] [PubMed] [Crossref]
- Milajerdi A, Abbasi F, Mousavi SM, Esmaillzadeh A. Maternal vitamin D status and risk of gestational diabetes mellitus: A systematic review and meta-analysis of prospective cohort studies. Clin Nutr. 2021;40(5):2576-2586. [Google Scholar] [PubMed] [Crossref]
- Morgan AS, Mendonça M, Thiele N, David AL. Management and outcomes of extreme preterm birth. bmj. 2022;376. [Google Scholar] [PubMed] [Crossref]
- Christoph P, Challande P, Raio L, Surbek D. High prevalence of severe vitamin D deficiency during the first trimester in pregnant women in Switzerland and its potential contributions to adverse outcomes in the pregnancy. Swiss Med Wkly. 2020;150(2122):w20238. [Google Scholar] [PubMed] [Crossref]
- Zisi D, Challa A, Makis A. The association between vitamin D status and infectious diseases of the respiratory system in infancy and childhood. Hormones. 2019;18(4):353-363. [Google Scholar] [PubMed] [Crossref]
- Lo TH, Wu TY, Li PC, Ding DC. Effect of Vitamin D supplementation during pregnancy on maternal and perinatal outcomes. Tzu Chi Med J. 2019;31(4):201-206. [Google Scholar] [PubMed] [Crossref]
- Mendes MM, Hart KH, Lanham-New SA, Botelho PB. Exploring the impact of individual UVB radiation levels on serum 25-hydroxyvitamin D in women living in high versus low latitudes: a cross-sectional analysis from the D-SOL study. Nutrients. 2020 Dec 11;12(12):3805. [Google Scholar] [PubMed] [Crossref]
- Lin S, Jiang L, Zhang Y, Chai J, Li J, Song X, Pei L. Socioeconomic status and vitamin D deficiency among women of childbearing age: a population-based, case–control study in rural northern China. BMJ open. 2021;11(3):e042227. [Google Scholar] [PubMed] [Crossref]
- Ahmed F, Khosravi-Boroujeni H, Khan MR, Roy AK, Raqib R. Prevalence and predictors of vitamin D deficiency and insufficiency among pregnant rural women in Bangladesh. Nutrients. 2021;13(2):449. [Google Scholar] [PubMed] [Crossref]
- Chang SW, Lee HC. Vitamin D and health-The missing vitamin in humans. Pediatr Neonatol. 2019;60(3):237-244. [Google Scholar] [PubMed] [Crossref]
- Janoušek J, Pilařová V, Macáková K, Nomura A, Veiga-Matos J, Silva DD, et al. Vitamin D: sources, physiological role, biokinetics, deficiency, therapeutic use, toxicity, and overview of analytical methods for detection of vitamin D and its metabolites. Crit Rev Clin Lab Sci. 2022;59(8):517-554. [Google Scholar] [PubMed] [Crossref]
- Urrutia-Pereira M, Solé D. Vitamin D deficiency in pregnancy and its impact on the fetus, the newborn and in childhood. Rev Paul Pediatr. 2015;33(1):104-113. [Google Scholar] [PubMed] [Crossref]
- Cui X, Gooch H, Petty A, McGrath JJ, Eyles D. Vitamin D and the brain: Genomic and non-genomic actions. Mol Cell Endocrinol. 2017 Sep 15;453:131-43. [Google Scholar] [PubMed] [Crossref]
- Judistiani RT, Nirmala SA, Rahmawati M, Ghrahani R, Natalia YA, Sugianli AK, et al. Optimizing ultraviolet B radiation exposure to prevent vitamin D deficiency among pregnant women in the tropical zone: report from cohort study on vitamin D status and its impact during pregnancy in Indonesia. BMC pregnancy and childbirth. 2019;19(1):209. [Google Scholar] [PubMed] [Crossref]
- Pereira-Santos M, Santos JY, Carvalho GQ, Santos DB, Oliveira AM. Epidemiology of vitamin D insufficiency and deficiency in a population in a sunny country: Geospatial meta-analysis in Brazil. Crit Rev Food Sci Nutr. 2019;59(13):2102-2109. [Google Scholar] [PubMed] [Crossref]
- Sunarno RD, Kartasurya MI, Suwondo A, Rahfiludin MZ. Vitamin D supplementation and sun exposure maintain blood pressures of pregnant women and increase birth weight in a randomized controlled trial. Iran J Public Health. 2023;52(10):2148. [Google Scholar] [Crossref]
- Ravinder SS, Padmavathi R, Maheshkumar K, Mohankumar M, Maruthy KN, Sankar S, Balakrishnan K. Prevalence of vitamin D deficiency among South Indian pregnant women. J Family Med Prim Care. 2022;11(6):2884-2889. [Google Scholar] [PubMed] [Crossref]
- Talukdar RK, Joshi SM. Vitamin D Status in Pregnant Women of North East India and Impact of Vitamin D Deficiency in Pregnancy on Feto-Maternal Outcome. Sch Int J Obstet Gynecol. 2019;8235:298-303. [Google Scholar] [Crossref]
- Jeyakumar A, Shinde V, Ravindran R. Pooled estimate of vitamin D deficiency among pregnant women in India: a systematic review and meta-analysis. J Health Popul Nutr. 2021;40(1):28. [Google Scholar] [PubMed] [Crossref]
- Özdemir AA, Gündemir YE, Küçük M, Sarıcı DY, Elgörmüş Y, Çağ Y, Bilek G. Vitamin D deficiency in pregnant women and their infants. J Clin Res Pediatr Endocrinol. 2018;10(1):44. [Google Scholar] [PubMed] [Crossref]
- Cabaset S, Krieger JP, Richard A, Elgizouli M, Nieters A, Rohrmann S, Quack Lötscher KC. Vitamin D status and its determinants in healthy pregnant women living in Switzerland in the first trimester of pregnancy. BMC pregnancy and childbirth. 2019;19(1):10. [Google Scholar] [PubMed] [Crossref]
- Mithal A, Kalra S. Vitamin D supplementation in pregnancy. Indian J Endocrinol Metab. 2014;18(5):593-586. [Google Scholar] [PubMed] [Crossref]
- Fogacci S, Fogacci F, Banach M, Michos ED, Hernandez AV, Lip GY, Blaha MJ, Toth PP, Borghi C, Cicero AF, Lipid and Blood Pressure Meta-analysis Collaboration. Vitamin D supplementation and incident preeclampsia: A systematic review and meta-analysis of randomized clinical trials. Clin Nutr. 2020;39(6):1742-1752. [Google Scholar] [PubMed] [Crossref]
- Mousavi SE, Amini H, Heydarpour P, Chermahini FA, Godderis L. Air pollution, environmental chemicals, and smoking may trigger vitamin D deficiency: Evidence and potential mechanisms. Environ Int. 2019;122:67-90. [Google Scholar] [PubMed] [Crossref]
- Shen Y, Pu L, Si S, Xin X, Mo M, Shao B, Wu J, Huang M, Wang S, Muyiduli X, Chen Z. Vitamin D nutrient status during pregnancy and its influencing factors. Clinical Nutrition. 2020 May 1;39(5):1432-9. [Google Scholar] [PubMed] [Crossref]
- Perreault M, Atkinson SA, Meyre D, Fusch G, Mottola MF, BHIP Study Team. Summer season and recommended vitamin D intake support adequate vitamin D status throughout pregnancy in healthy Canadian women and their newborns. J Nutr. 2020;150(4):739-46. [Google Scholar] [PubMed] [Crossref]
- Kumar KJ, Chavan A, Shushma K, Murthy S. Comparison of vitamin D status between urban and rural south Indian mothers and their newborns. J Nepal Paediatr Soc. 2016;36(3):243-249. [Google Scholar] [Crossref]
- Chávez-Courtois M, Godínez-Martínez E, Muñoz-Manrique C, Negrete-Martínez V, González-Leyva CP, Tolentino-Dolores M, et al. Vitamin D status and its determinants in Mexican pregnant women from a rural and an urban area: a comparative study. Int J Environ Res Public Health. 2021;18(9):4571. [Google Scholar] [PubMed] [Crossref]
- Wei SQ, Bilodeau JF, Julien P, Luo ZC, Abenhaim HA, Bi WG, et al. Maternal vitamin D, oxidative stress, and pre‐eclampsia. Int J Gynaecol Obstet. 2021;154(3):444-450. [Google Scholar] [PubMed] [Crossref]
- Woo J, Giurgescu C, Wagner CL. Evidence of an association between vitamin D deficiency and preterm birth and preeclampsia: a critical review. J Midwifery Womens Health. 2019;64(5):613-629. [Google Scholar] [PubMed] [Crossref]