DESCRIPTION
Primary health care refers to a multidisciplinary team having expert knowledge and skills on COVID-19's impact arose from its rapid emergence, the number of people needing intensive care, and presented many clinical problems, including respiratory failure, excessive immunological response and clotting disorders, renal failure and myocarditis [1]. Knowledge of the disease process and which tissues are likely to have been damaged is important in the health care process [2].
After COVID-19, a patient may develop persisting dysfunction of almost any organ and experience well-established direct (physical) and indirect (psychological) effects associated with severe illness and a long stay in an intensive care unit [3]. The majority of patients will need pulmonary care which is usually a separate service attached to a respiratory medicine department.
For patients with ventilator dependence, diaphragmatic dysfunctions are very common, often causing difficult weaning, and may result in secondary infections and extended hospital stays.
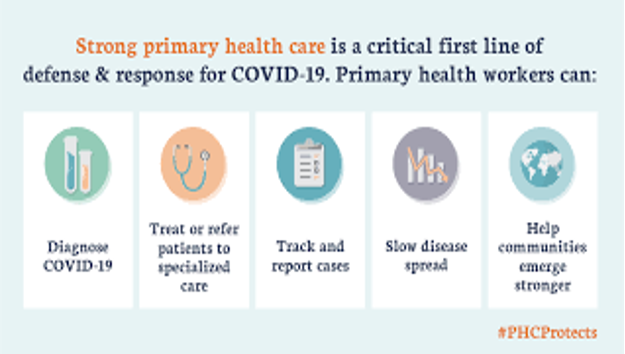
Figure: Role of Primary Health Care in COVID-19 Response
In the care of diaphragm dysfunction, a diaphragm pacemaker is more commonly used. Clinical trials have shown that the use of an external diaphragm pacemaker can effectively increase diaphragm muscle strength and endurance in ICU patients.
Exercise that uses muscles and increases demand upon the cardio-respiratory system will be important and should be encouraged from the outset [4]. Malnutrition can prolong infection healing times and increase the length of hospital stay and nutritional support for patients with COVID-19 also influences disease progression. COVID-19 is predicted to challenge in health care with many more patients needing longer-term complex care input and will continue to do so for at least few years.
Large numbers of people are surviving COVID-19 after quite severe illness and will present with a mixture of cardio-respiratory, mental health, and neuromuscular problems, will need local, community-based internal organisation, warrant a team within the health care system who would develop specific expertise in the care of people [5].
CONCLUSION
Primary health care is central to managing the long-term impacts of COVID-19. The disease’s rapid onset and severity have overwhelmed many healthcare systems. Patients often suffer from multi-organ dysfunction, including respiratory and cardiac issues. Knowledge of affected tissues and systems is vital for effective patient care.
Post-COVID conditions may include respiratory failure, myocarditis, renal complications, and clotting disorders. Pulmonary care, especially for ventilator-dependent patients, is frequently required. Diaphragmatic dysfunction is common and may delay recovery and hospital discharge. Diaphragm pacemakers have shown promise in improving muscle function in ICU patients.
Exercise should be encouraged early to enhance cardiorespiratory recovery. Nutritional support is also crucial, as malnutrition can hinder healing and prolong hospitalization. Mental health support is needed due to psychological effects from ICU stays. COVID-19 survivors often require long-term, multidisciplinary care strategies.
A coordinated approach across specialties ensures better outcomes and faster recovery. Community-based healthcare teams must develop expertise in post-COVID care. The pandemic's lasting effects demand an adaptable and integrated primary health care system.
REFERENCES
- Muthiah R. (2021) Isolated Acute Rheumatic Pancreatitis A Case Report. Case Reports in Clinical Medicine. 10, 52-77. [
Google scholar ] - Muthiah R. (2019) Infective Endocarditis in Tetralogy of Fallot Complicating Brain Abscess A Case Report. Case Reports in Clinical Medicine. 8, 105-126. [
Google scholar ] - Muthiah R. (2018) Native Aortic Valve Endocarditis A Case Report. Case Reports in Clinical Medicine.7, 483-504. [
Google scholar ] - Muthiah R. (2018) Tropical Coronary Artery Disease and Arrhythmogenic Potentials The Changing Pattern towards Endomyocardial Fibrosis An Analysis. Case Reports in Clinical Medicine. 7, 397-429. [
Google scholar ] - Muthiah R. (2018) Isolated Patent Ductus Arteriosus in an Elderly Female, Aged 65 Years A Case Report. Case Reports in Clinical Medicine.7, 352-379. [
Google scholar ]